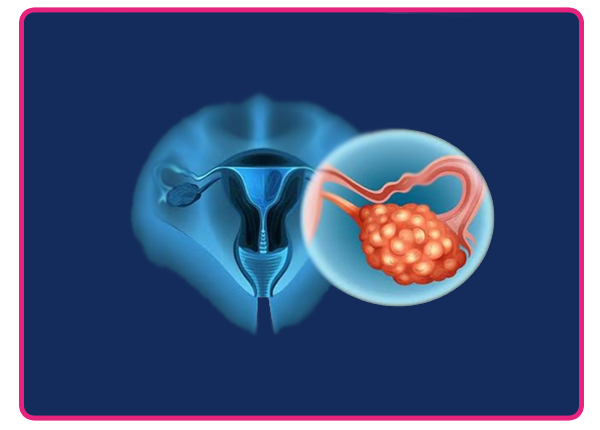
Ovarian Cancer Treatment
Fatal variant with high proliferative activity. Includes high grade variants of serous, endometrioid, carcinosarcoma, undifferentiated carcinoma. Arise from STIC (serous tubal intraepithelial cancer).
RISK FACTORS
1. Age: postmenopausal
2. nulliparous
3. Family history: strongest risk factor
4. Late menopause, early menarche
5. Protective factors: multiparity, OCP use, tubal ligation, hysterectomy, BSO, lactation
PATHOLOGY
Three main types:
1. Epithelial (95%): serous, mucinous, endometrioid, clear cell, transitional cell, undifferentiated
2. Germ cell(3-4%): dysgerminoma, yolk sac tumour, teratoma, embryonal, choriocarcinoma, mixed
3. Stromal cell (1%): granulosa cell, sertoli-leydig cell tumour
DIAGNOSIS
- History & physical examination: history of nonspecific gastrointestinal complaints like nausea, dyspepsia, altered bowel habits, abdominal distension due to ascites.
- Tumour markers: CA125 ( may be elevated in non malignant conditions, less frequently elevated in mucinous, clear cell and borderline tumours), LDH (dysgerminoma), HCG(choriocarcinoma), AFP( yolk sac tumour)
- Imaging: CT/MRI/PETCT (metastatic work up)
TREATMENT
- SURGERY: Mainstay of treatment. Aim is complete cytoreduction with hysterectomy, removal of tubes and ovaries, lymph node evaluation, omentectomy, peritoneal stripping. May include intestinal resection, stoma formation, splenectomy, urinary diversion.
- CHEMOTHERAPY: Platinum based, most commonly combination of carboplatin & paclitaxel (three weekly). For germ cell tumours- BEP (bleomycin, etoposide, cisplatin).
- RADIATION THERAPY: For oligometastatic recurrent disease.
Category:Ovarian Cancer Treatment