Cervical Cancer Treatment
CERVICAL CANCER
Cervical cancer is the most common gynecologic cancer in women globally. In low and middle income countries, it is more common. About 75-85% are from developing countries.
ETIOLOGY
Persistent HPV infection is the main cause of cervical cancer. More than 150 types of HPV have been described, out of which HPV 16 and 18 account for 80% cases.
RISK FACTORS
- Lack of regular cervical screening
- High risk seual behavior
- Early coitarche (age at first coitus,<20 years)
- Early marriage
- Multiple child births
- Frequent change of partners
- Having a male partner with multiple sexual partners
- Smoking
- Low socio-economic status
- Low immunity
- Age: bimodal peak- 30-39 and 60-69years.
PREVENTION
- Screening by cytology (PAPs smear) every three years or HPV DNA testing every 5 years starting at 25 years of age.
- Vaccination: girls 9-13 years- Gardasil, Cervarix
PATHOLOGY
The main histological types of carcinoma cervix are: 1. Squamous cell (85-90%) 2. Adenocarcinoma 3. Mixed 4. Neuroendocrine 5. Others
CLINICAL PRESENTATION
- Asymptomatic (early stages)
- Vaginal bleeding- irregular, intermenstrual, post-coital, postmenopausal
- Vaginal discharge- copious, purulent, malodorous
- Cachexia
- Micturition symptoms- dysuria, frequency, urinary incontinence (VVF)
- Rectal symptoms- rectal pain
- Pain- dyspareunia, low backache, deep pelvic ache, sciatica.
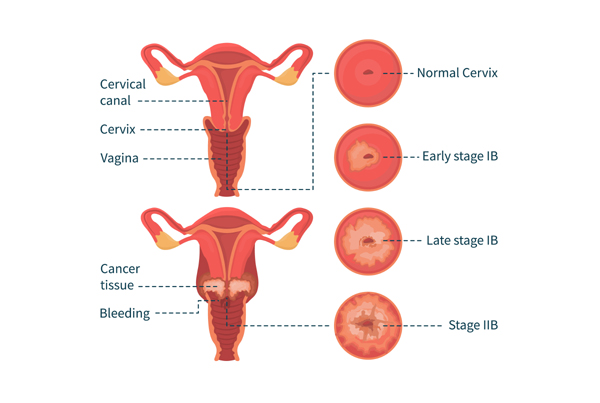
DIAGNOSIS
- History & physical examination
- Invesigations: PAPs smear, colposcopy, cervical biopsy, MRI (best imaging modality), PET/CT (metastatic work up), cystoscopy and proctoscopy (if symptoms are suggestive)
TREATMENT
- SURGERY: Treatment of choice in early stages- stage IA, IB1,IB2, IIA1- radical hysterectomy + B/L PLND.
- FERTILITY PRESERVATION: simple trachelectomy/ conisation- stage IA1 (without LVSI), radical trachelectomy + B/L PLND- stage IA1 (withLVSI), IA2, IB1
- CONCURRENT CHEMORADIATION: stage IB3, IIA2 (bulky disease), IIB-IVA
Category:Cervical Cancer Treatment